Visby Coding Guide for STD Testing
Coding Guide for STD testing regarding Gonorrhea, Chlamydia and Trichomonas
Sexually transmitted infections (STI) consist of N. gonorrhoeae (gonorrhea) and C. trachomatis (Chlamydia) which are highly prevalent in the family of sexually transmitted disease (STD). There were nearly 68 million infections in 2018 (prevalence), and that 1 in 5 people in the U.S. have an STI. The graphic also shows that there were 26 million STIs acquired in 2018 (incidence). The direct lifetime medical costs of new STIs in 2018 totaled nearly $16 billion (in 2018 dollars). Gonorrhea is a common STI and the CDC estimates approximately 1.6 million new gonorrhea infections occurred in the United States in 2018 with more than half occurring among young people aged 15-24.[1] Chlamydia is also a common STD that infects both men and women and can cause serious permanent damage to a woman’s reproductive system making it difficult for her to get pregnant and can also cause a potentially fatal ectopic pregnancy.
Testing
Testing is key in the prevention of the spread of STDs in both men and women who are sexually active. Testing can be accomplished either through urine sample or cotton swab sample from the vagina. Persons with HIV infection should be screened annually if sexually active and more frequently (three-to-six month intervals) for men who have sex with men (MSM), particularly for those with multiple partners. Under-treatment and/or delayed treatment of an STD can and often does result in significant consequences for the patient. The transmission of an STD pathogen continues for the sexually active patient; complications of an untreated progressive infection can include pelvic inflammatory disease with risk of infertility, ectopic pregnancy and/or chronic pelvic pain. For the provider, there is no guarantee the patient will return, staff increases work-flow to contact patient for return for treatment, and neither patient or clinician are satisfied with the outcome.
In some cases the clinician elects to treat the patient before lab results are provided so the patient is treated for “possible” infection that may not be present thus resulting in unnecessary medication that may have adverse effects, chance of increasing antibiotic-resistant infections, loss of confidence in clinician’s decision making when treating a non-existent infection, additional strain on staff work flow to reschedule for correct treatment, and reduced patient and clinician satisfaction.
Treatment
According to the CDC, “in settings where same-day treatment is available for patients with STD-related conditions and for sex partners of patients with a diagnosed STD, treatment should not be delayed while awaiting diagnostic test results. Delays in treatment might increase complications and contribute to transmission of infection in the community; and same-day treatment has numerous public health benefits. In an STD specialty care setting, same-day treatment should take place on site with the provision of a full course of appropriate medication. The first dose should be administered while the patient is in the clinic.”
Insurance Coverage for Testing and Treatment
Medicare Part B (Medical Insurance) covers sexually transmitted infection (STI) screenings for chlamydia, gonorrhea, syphilis, and/or Hepatitis B if you’re pregnant or at increased risk for an STI. Medicare also covers up to two face-to-face, high-intensity behavioral counseling sessions if you’re a sexually active adult at increased risk for STIs. Each session can be 20-30 minutes long. Medicare covers STI screenings once every 12 months, or at certain times during pregnancy. Medicare covers up to two behavioral counseling sessions each year.
Private payers have individualized coverage based on employer options plan internal coverage options. According to the CDC, the affordable care act (ACA) includes provisions aimed at improving coverage of, and access to certain preventive health services. The following plans cover testing without cost-sharing.
- Non-grandfathered private health insurance plans
- Medicare
- Medicaid expansion plans (optional for adults, depending on state policy. Often covered for children)
- Traditional Medicaid plans
Overview of Relevant Reporting Codes
Preventive Medicine
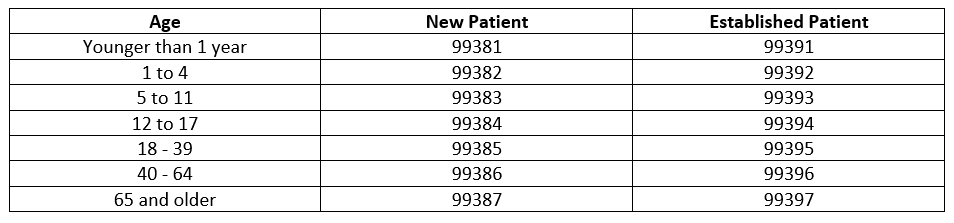
Preventive medicine codes (New 99381-99387), (Established 99391-99397) are used to report the preventive medicine evaluation and management of infants, children, adolescents, and adults. If an abnormality is encountered or a preexisting problem is addressed in the process of performing this service and it is significant enough to require additional workup requiring the key components of an E/M service, the office/outpatient codes should be reported with modifier -25 (CPT 2023).
2023 CODE TABLE; PREVENTIVE MEDICINE SERVICES
Documentation
Documentation by providers must include whether the patient is New or Established, age of patient, complete, pertinent history and physical examination, orders for testing and treatment, risk factors from findings, differential diagnoses if pertinent, and referral.
Diagnosis findings should be documented to include conclusions following testing, additional problems managed at the visit and co-existing problems either being managed concurrently by the treating physician or those that exist and will be managed on follow-up to another physician and/or specialist.
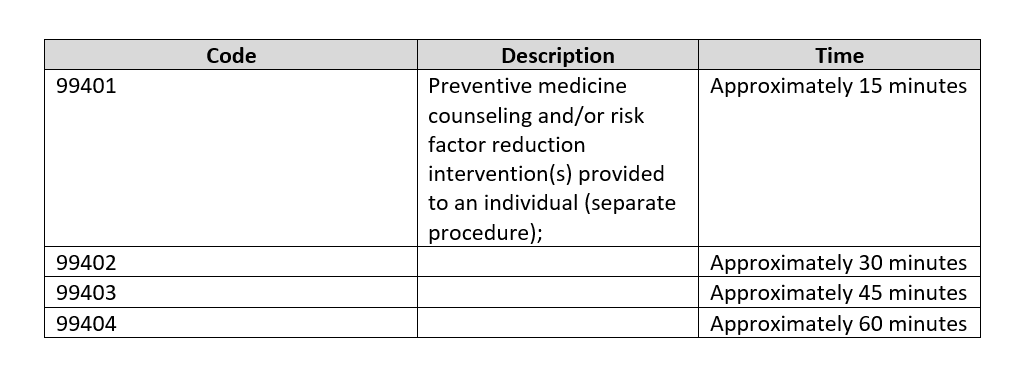
Counseling Risk Factor Reduction and Behavior Change Intervention
Counseling for Risk Factor Reduction and Behavior Change Intervention are used to report services provided face-to-face by a physician or other qualified health care professional for the purpose of promoting health and preventing illness or injury. If billed in addition to evaluation and management codes, the -25 modifier would be appended to the E/M level. See CPT 2023 for additional descriptors.
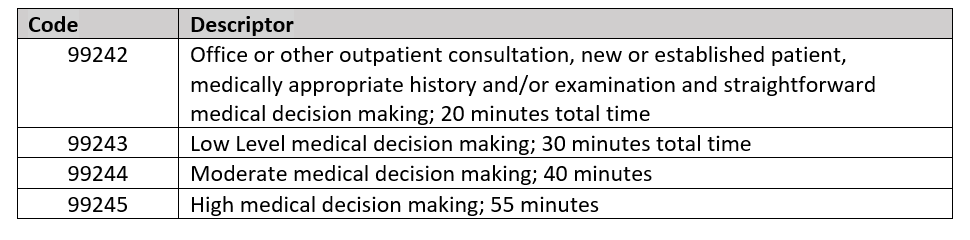
Counseling Codes for Office or Other Outpatient Consultations
Counseling codes can be used for the initial consultation for a specific problem when referred by another provider. Any follow-up services related to the specific problem provided by the consulting physician are billed with the appropriate outpatient visit codes.
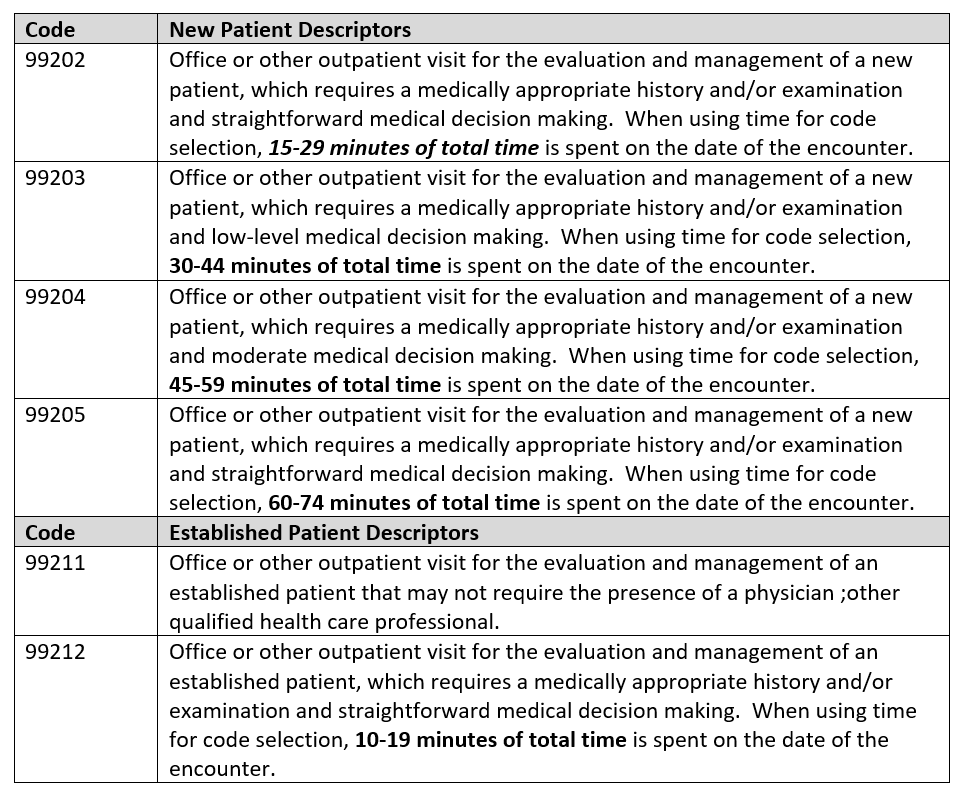
2023 Content of CPT Evaluation and Management Service Codes
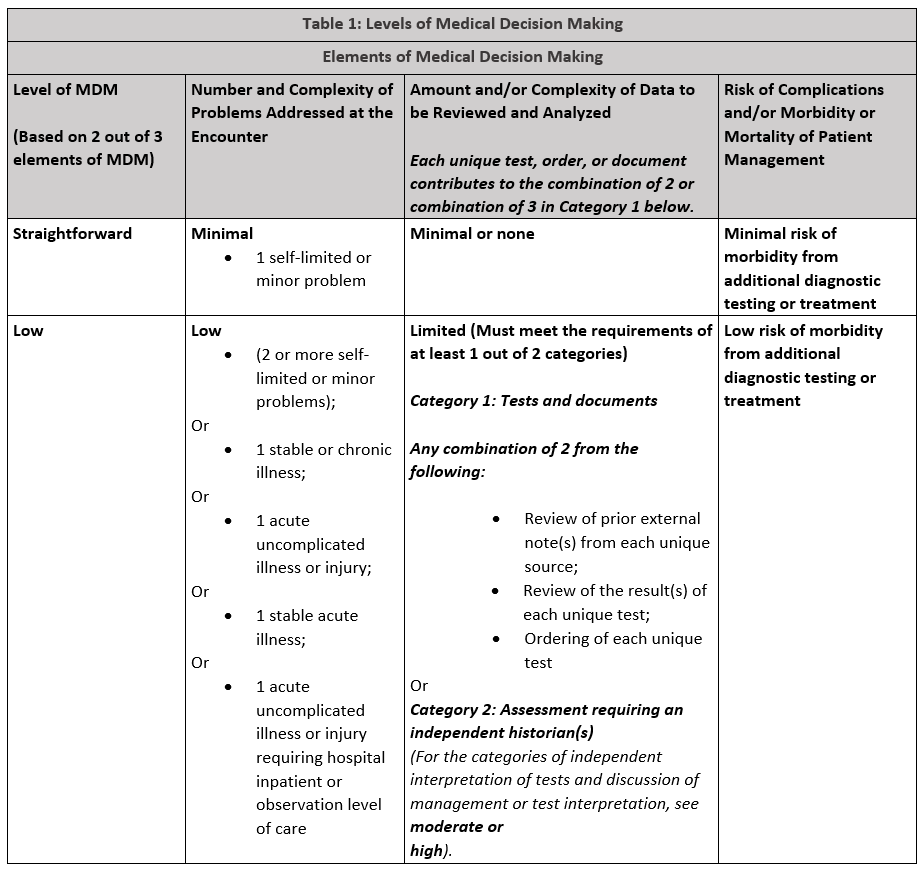
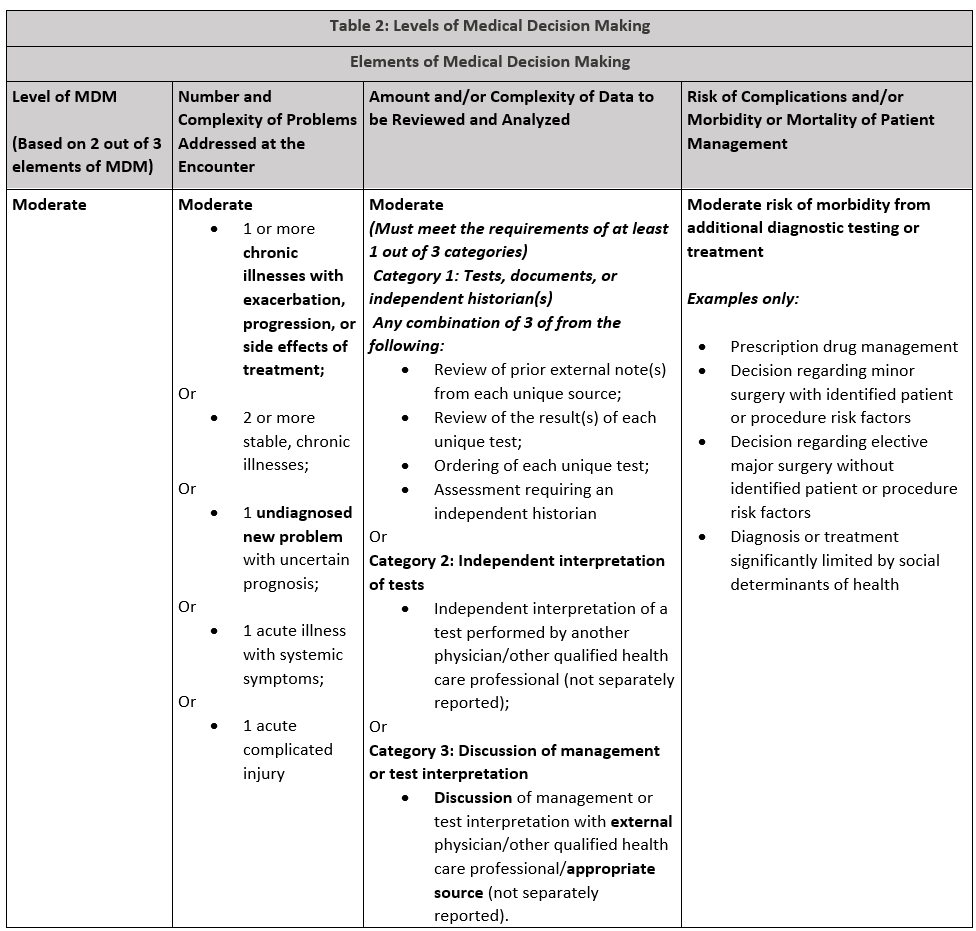
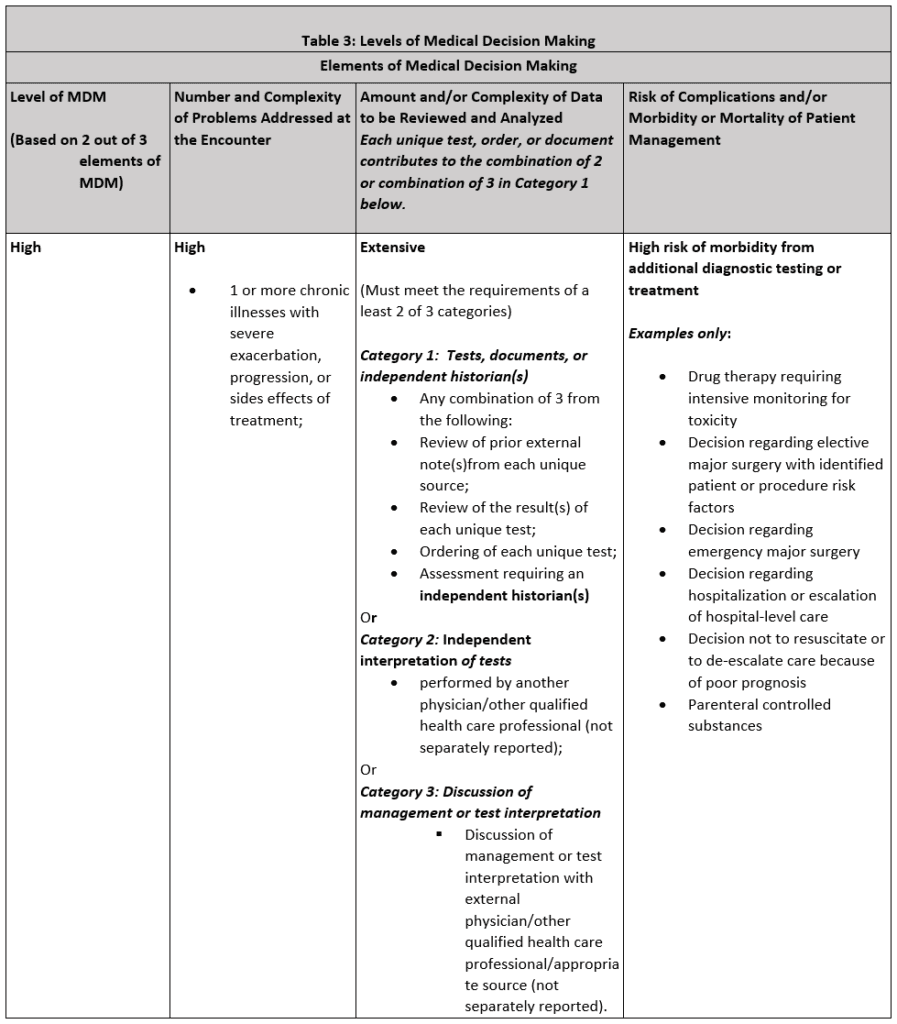
The E/M code descriptors were modified by the American Medical Association for revision in 2022 and 2023. There were extensive changes made in how the final code level is chosen which recognizes the level of Medical Decision Making or Time, depending on the code set, as the determinant of the code choice. History and Physical Examination are required to be “medically appropriate” but are not calculated in the final code choice. For outpatient office/clinic visits, either Medical Decision Making or Time determine the code billed. Times range from
New Patient
The CPT definition of “New Patient” is one who has not received any professional services from the physician or other Qualified Health Care Professional (QHCP) or another physician or QHCP of the exact same specialty and subspecialty who belongs to the same group practice withing the past three years.
Established Patient
The CPT definition of “Established Patient” is one who has received professional services from the physician or other qualified health care professional or another physician or other QHCP of the exact same specialty and subspecialty who belongs to the same group practice within the past three years.
Consideration of Time in E/M Levels
Time is not a consideration for coding emergency department E/M levels but it will be for most other E/M levels. Note the times listed in each table for appropriate time requirements must be supported by documentation in the medical record.
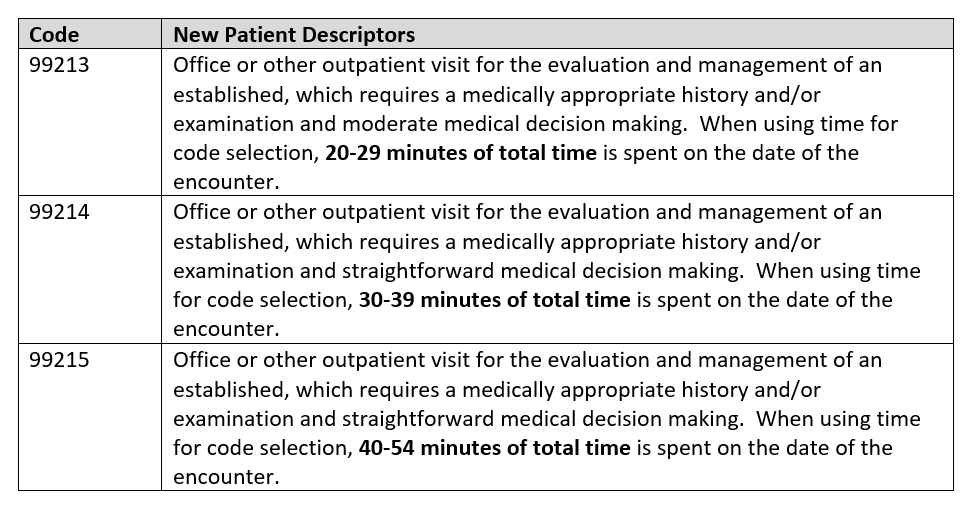
Office or Other Outpatient Services
Emergency Department Services
As of January 1, 2023, The emergency department evaluation and management codes to not distinguish new or established patients nor do they recognize total time spent on the date of the encounter. These codes are used by the emergency medicine provider scheduled in the ED. For other providers seeing patients in the ED, the office or other outpatient service codes are used. Emergency medicine evaluation and management levels are determined by two of three medical decision making components that meet or exceed the requirements of the level.
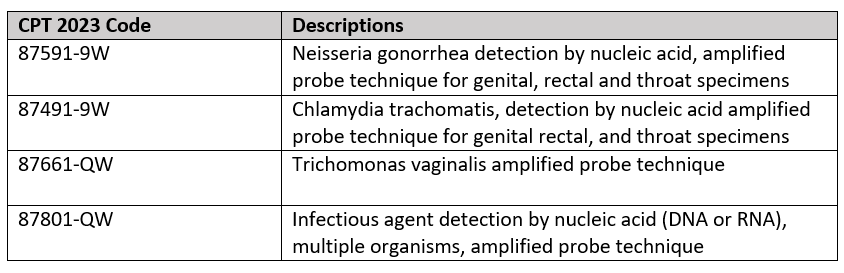
Selecting the appropriate Laboratory CPT Code
Whether or not the clinic bills independently for the labs used to diagnose chlamydia and gonorrhea specimens, it is important to assure the lab CPT codes are billed correctly. Following are codes pertinent to Gonorrhea and Chlamydia testing:
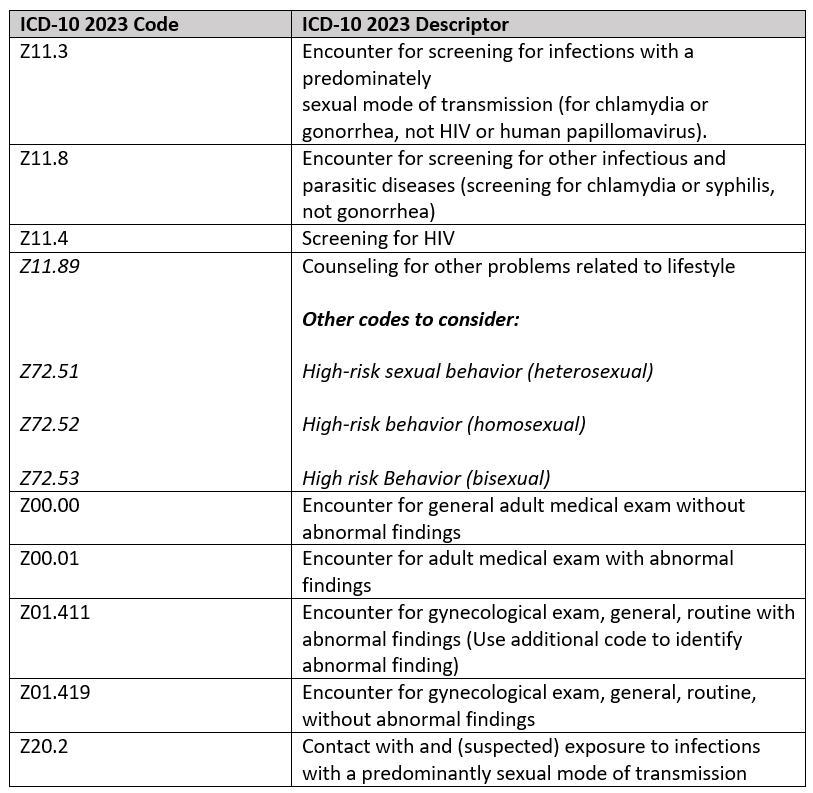
SELECTED STI SCREENING PREVENTIVE ICD-10 DIAGNOSIS Z-CODES 2023
According to the CDC in 2020, “Screening and diagnostic testing are important to detect asymptomatic or confirm suspected infections. Previous studies have documented that one third to one half of primary care clinicians routinely screen men or women for STDs (chlamydia, gonorrhea, syphilis, or HIV) (26,33,38,39). Obstetricians-gynecologists screen nonpregnant women more often than other primary care physicians (39–41). Community health centers often provide routine HIV testing for pregnant women but less frequently offer routine HIV testing for men and nonpregnant women (42,43). Some emergency departments perform routine HIV testing, although the practice is not widespread (44). For correctional settings, routine testing varies by type of facility. State and federal prison systems commonly perform routine syphilis testing at intake but less often offer routine testing for HIV, gonorrhea, or chlamydia (45). Some city and county prisons conduct routine testing for syphilis but rarely offer routine testing for HIV, gonorrhea, or chlamydia (45). Jails and juvenile detention centers infrequently offer routine testing for STDs and rarely perform routine HIV testing (46,47).”
Asymptomatic Coding for STI
The following codes identify STI screening and preventive diagnosis coding opportunities for 2023. Note some code descriptors have minimal changes from prior years. These codes are to be used for testing for a disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those that test positive for the disease. One cannot emphasize the importance of including ALL pertinent diagnosis codes to provide a total picture of the patients’ problems managed at the encounter.
Signs and Symptoms that Impact Coding for STDs
Often patients see their physician, go to an Emergency Department or Urgent Care Center complaining of symptoms consistent with an STD. Following are some of the complaints consistent with suspicion of STD:
For females:
- Genital itchiness
- Lumps and bumps in the vulva and vagina
- Changes in vaginal discharge
- Pain in the affected area
- Lower abdominal pain
- Pain during intercourse or urination
For males:
- Unusual discharge from the penis
- Lumps or bumps on the genital area
- Sores or ulcers on the genital area
- Burning or pain during urination
- Pain in the lower abdomen
- Pain during sex or ejaculation
- Painful or swollen testicles
These are visits that are billable based on the location where care is sought. For the Office, Codes 99202-99205 (New patient) or 99211 – 99215 (established patient) would be appropriate for the overall examination and treatment. The laboratory tests would be billed separately and assigned the code consistent with the type of test. If the site of service is the ED, Codes 99281-99285 would be appropriately billed by the provider and the hospital would bill for the technical service using the 99281-99282 codes as well as the laboratory codes.
Preventive Medicine Services (99381-99387) New patient, (99381 – 99397) Established patient, are examinations without symptoms but scheduled to identify risks and prevent a number of conditions. For example, a patient who is notified they have been exposed to an STD. Once a condition is identified during the preventive Medicine visit, labs may be ordered and additional visits may be necessary. When this occurs, the next visit would cease to be preventive and fall under the appropriate Office or Urgent Care service level and any labs would be billed separately.
Counseling Risk Factor Reduction and Behavior Change Intervention (Preventive Medicine, Individual Counseling (99401 – 99404) are time-based codes used to promote health and prevent illness or injury. These codes are used for individuals without a specific illness for which the counseling might otherwise be used as part of treatment. They would include family problems, diet and exercise, substance use, sexual practices, injury prevention, dental health and diagnostic and laboratory test results available at the time of the encounter for review and discussion.
Coding Technique Example
20 year-old college student known to the practice schedules a visit with concerns relating to unprotected sex recently. Patient collects a vaginal swab sample testing is performed prior to the exam. Patient is examined including pelvic examination. Exam and on-site STI lab results indicate patient is positive for Chlamydia. Results reviewed with patient then patient received ceftriaxone (Rocephin) 250 mg given intramuscularly and Azithromycin (Zithromax) is given orally. Patient is counseled and advised to return for recheck in ten days.
Codes Assigned
CPT Procedure Codes:
99204-25 New patient office service
87801 Infectious agent, multiple organisms
96372 Therapeutic, prophylactic, or diagnostic injection (specify substance or drug); subcutaneous or intramuscular.
XXXXX Identify the substance injected
ICD-10 Diagnosis Codes:
Z70.2 Other specified counseling
Z11.3 – Encounter for screening for infections with a predominately sexual mode of transmission
Z72.51 High risk sexual behavior (heterosexual)
Example 2:
22 year-old female admits to unprotected sex 1 week ago and wants to be tested for STD although asymptomatic at this time. Patient is currently homeless. Patient conducts self-collected swap on arrival. Physical examination includes pelvic examination and STI panel is positive for Trichomonas. Patient is prescribed metronidazole (Flagyl®), counseled on prevention and discharged. Provider spends 35 minutes in attendance to the patient including counseling and discussion of lab results.
CPT Procedure Codes
99204-25 New patient office service (undiagnosed new problem with uncertain prognosis, prescription drug management; treatment significantly limited by social determinates of health (homelessness, inability to afford medication)
87801 Infectious agent, multiple organisms
ICD-10 Diagnosis Codes:
A59.00 -Urogenital trichomoniasis, unspecified
Z11.3 – Encounter for screening for infections with a predominately sexual mode of transmission
Z72.51 High risk sexual behavior (heterosexual)
K62.89 Other specified counseling
References and Additional Reading:
Gonorrhea-CDC Detailed Fact Sheet: https://www.cdc.gov/stdfact-gonorrhea-detailed.htm
CDC STD Fact Sheets: https://www.cdc.gov/std/healthcomm/fact_sheets.htm
CDC: Sexually Transmitted Disease Preventive Services Coverage: https://www.cdc.gov/std/healthcomm/fact_sheets.htm
Medicare/CMS: https://www.medicare.gov/coverage/sexually-transmitted-infection-screenings-counseling
CDC Sexually Transmitted Diseases: https://ww.cdc.gov/nchhstp.newsroom/2021/2018-STI-Incidence-prevalence-estimates.html.
CDC: https://www.chlamydiaexplained.com/what-is-the-best-treatment-for-gonorrhea-and-chlamydia/
Drugs.com: https://www.drugs.com/medical-answers/antibiotics-treat-chlamydia-gonorrhea-3121689/
National Library of Congress: Diagn Microbiol Infect Dis. 1993 Feb;16(2):165-72. doi: 10.1016/0732-8893(93)90016-z.
Chlamydia trachomatis by Amplified Probe Technique: https://www.uwhealth.org/lab-test-directory/microbiology/name-67808-en.html; UWHC Laboratory Services: Microbiology
Trichomonas Facts: https://www.cdc.gov/std/trichomonas/STDFact-Trichomoniasis.htm
STD Treatment: https://www.cdc.gov/std/treatment/default.htm
CDC Trichomoniasis Treatment: https://www.cdc.gov/std/treatment-guidelines/trichomoniasis.htm
Trichomoniasis Treatment: https://my.clevelandclinic.org/health/diseases/4696-trichomoniasis
ICD-10 Data: https://www.icd10data.com/ICD10CM/Codes/A00-B99/A50-A64/A59-/A59.9
CPT 2023: Professional Edition, American Medical Association; Copywrite 2022
Chlamydia testing and treatment: https://www.chlamydiaexplained.com/
Posted by: Vicky Damours on 2/9/23
© 2026 - Edelberg & Associates

