News
Hospitals and physician practices are increasingly affected by overwhelming number of payer denials without basis. Initially these denials affected primarily physician billing but of late, they have expanded to the facility portion of the ED charge and present growing challenges for hospitals struggling to staff their RCM departments to handle the constantly increasing numbers. When attempting to manage denials, a general “roadmap” can be effective to address the details supporting provider selection of charge codes. A review of the best content elements can assist in providing payers with undeniable support for the services rendered.
Content of Facility Coding Criteria
The Federal Register (Vol. 68, No. 155, p. 63461 -48008 -48010) outlined the Medicare conditions for charging the Facility component of an ED visit as follows, “Facilities code clinic and emergency department visits using the same (Physicians) Current Procedural Terminology codes as physicians. For both clinic and emergency department visits, there are currently five levels of care (99281-99285) plus Critical Care (99291-99292). Because these codes are defined to reflect only the activities of physicians, they are inadequate to describe the range and mix of services provided by the hospital to patients in the clinic and emergency department settings (for example, ongoing nursing care, preparation for diagnostic tests and patient education).” This would establish the need for separate identification of ED Facility leveling separate and distinct from professional E/M leveling.
In the April 7, 2000 final rule (65 FR 18434), CMS gave each facility the responsibility to create an internal set of guidelines to determine the visit (E/M) level for each patient. CMS stated that hospitals should develop criteria for outpatient visits that meet the following criteria announced in the August 9, 2002 proposed rule (67 FR 52131):
- Coding guidelines for emergency and clinic visits should be based on emergency department or clinic facility resource use, rather than physician resource use.
- Coding guidelines should be clear, facilitate accurate payment, be usable for compliance purposes and audits, and comply with HIPAA.
- Coding guidelines should only require documentation that is clinically necessary for patient care. Preferably, coding guidelines should be based on current hospital documentation requirements.
- Coding guidelines should not create incentives for inappropriate coding.
The American College of Emergency Physicians (ACEP) developed an emergency department facility coding criteria that is currently in use at a majority of U.S. Hospitals and has become the model of ED facility code assignment. However, payers often utilize proprietary facility coding criteria to approve or deny ED claims without sharing that information with their participating providers which make it increasing difficult to identify why, specifically, payment for claims is downcoded or denied.
Medical Necessity
It is not uncommon to see claims downcoded for lack of medical necessity which is a subjective concept that can be utilized by payers to downcode or deny payment for submitted claims. The American Academy of Professional Coders (AAPC) notes that CMS allows its Medicare Administrative Contractors (MACs) to determine whether services provided to their beneficiaries are reasonable and necessary, and therefore medically necessary. MACs use the following criteria to determine if an item or service is medically necessary:
- It is safe and effective.
- It is not experimental or investigational.
- It is appropriate when:
- Furnished in accordance with accepted standards of medical practice.
- Furnished in a setting appropriate to the medical needs and condition.
- Ordered and furnished by qualified personnel.
- Meets the medical need of the patient.
Note: There are some exceptions to the general medical necessity requirements spelled out in CMS’ regulations.
EMTALA (Emergency Medicine Treatment and Labor Act)
First it is necessary to recognize the standards outlined by EMTALA. According to CMS, Congress enacted the Emergency Medical Treatment & Labor Act (EMTALA) in 1986 “to ensure public access to emergency services regardless of a patient’s ability to pay. Section 1867 of the Social Security Act imposes specific obligations on Medicare-participating hospitals that offer emergency services to provide a medical screening examination (MSE) when a request is made for examination or treatment for an emergency medical condition (EMC), including active labor, regardless of an individual’s ability to pay. Hospitals are then required to provide stabilizing treatment for patients with EMCs. If a hospital is unable to stabilize a patient within its capability, or if the patient requests, an appropriate transfer should be implemented.”
“Emergency medical services” means the delivery of health care services under emergency conditions occurring as the result of a patient’s condition due to a work injury that manifests itself by symptoms of sufficient severity, including severe pain, such that a prudent layperson, who possesses an average knowledge of health and medicine, could reasonably expect the absence of immediate medical attention to be life-threatening or cause serious harm or aggravation of physiological or psychological sickness, injury, or incapacitation.”
According to CMS, Congress enacted the Emergency Medical Treatment & Labor Act (EMTALA) in 1986 “to ensure public access to emergency services regardless of ability to pay’. Section 1867 of the Social Security Act imposes specific obligations on Medicare-participating hospitals that offer emergency services to provide a medical screening examination (MSE) when a request is made for examination or treatment for an emergency medical condition (EMC), including active labor, regardless of an individual’s ability to pay. Hospitals are then required to provide stabilizing treatment for patients with EMCs. If a hospital is unable to stabilize a patient within its capability, or if the patient requests, an appropriate transfer should be implemented.”
Medical Screening Examination and Emergency Medical Conditions
EMTALA obligates Medicare participating hospitals to provide a medical screening examination when a patient presents to the emergency department for examination or treatment of an emergency medical condition (EMC). Until the medical screening examination is provided, hospitals may not query the patient about insurance or payment, formerly referred to as a “wallet biopsy”. Unfortunately, EMTALA is an unfunded federal mandate with the greatest responsibility placed on the hospitals and emergency physicians who provide this care shouldering the financial burden of providing EMTALA related medical care regardless of whether payment is made, according to the EMTALA Fact Sheet prepared by the American College of Emergency Physicians.
Presenting Problem vs. Final Diagnosis in Emergency Conditions
Many insurance plans are currently retrospectively denying claims for emergency departments visits by basing the determination of an emergency on a patient’s final diagnosis/medical necessity, rather than the presenting problems/symptoms. This is in direct conflict with EMTALA which requires at least a medical screening exam, including diagnostic studies until a medical emergency has been ruled out.
Outlining Components of Emergency Department Treatment Denial Reconsideration
- Summarize the reason for the reconsideration request by outlining how the originally billed code met details of code requirements, what conditions and/or treatment(s) were primary and why.
- Restate the patient demographic information and reason for visit
- Restate major patient past medical history that may be creating problems now
- Discuss the physician’ major findings from physical examination
- Detail the differential diagnosis and establish how it effects the ordering of diagnostic studies and medications
- Provide a brief description of the course of treatment in the ED and focus on any problems, modifications to medications and patient response to treatment
- Discuss how treatment meets the standards of practice for the problems being addressed. The specialty of emergency medicine has many textbooks and articles that address standards of practice and the importance can never be stressed enough.
- Summarize any findings and discussions with other providers and note their impressions and specialty of consultant
- Discuss any documented nurses notes, cautions, concerns, patient responses to treatment of any kind, changes in therapy and family concerns
- Provide discussion of Discharge orders, location, concerns for future patient care and family concerns and limitations on care provision if pertinent.
- If pertinent, discuss Chief Complaint and presenting problems vs. final diagnosis and decisions for discharge, transfer, admission and/or observation stay
- If available, compare to information on other claims that resulted in payment and stress inconsistencies in decision making by the payer
The revenue cycle industry is undergoing significant challenges as payers take advantage of the new coding system to drive down payments. This has resulted in significant volumes of denials that must be managed individually in order to receive at least partial payment for denied claims. In addition, the Emergency Medicine industry has been frothed with significant challenges as more and more uninsured presents to the Emergency Department for treatment and significant numbers of patients remain in Emergency Departments for extended periods of times, often days, with no easy or established mechanism for billing and receiving payment for these unique situations.
The American Medical Association (AMA) continues to revise coding descriptors to address these changes, but payers are slow to pick up on these and continue to deny services that don’t fit into their specialized programs. It is important that several conditions exist in order to assure:
-
- Number One accurate coding,
-
- Number Two complete documentation by providers,
-
- Number Three accurate billing and,
-
- Number Four attention to payments, reasons for denials, and management of resubmission of claims.
With regards to coding, first things first, coding companies should have errors and omissions insurances to cover any significant coding errors that occur.
With “payor based” coding, this leaves coding companies open to and vulnerable to accusations of coding errors. For examples, CPT has certain coding rules published. Medicare has different clarifications of these coding rules. In addition, Medicare also has numerous Medicare carriers that interpret rules differently; some see things one way, some see things another, so coding company must adhere to local MAC rules to assure accurate coding.
Medicaid and private payors have their own interpretations that are often not published; therefore it is very difficult for coding to be performed accurately without specific rules to follow when they exist. This is why denial management is so critically important. Fortunately, there are not as many rules for Emergency Medicine as there are for other specialties, and so the risk is limited.
By far the biggest challenge is working within payor guidelines and managing extensive denials for payment. Payment denials don’t mean that inaccurate coding has taken place. It is important to know what interpretations of National Guidelines coding companies are following. For examples, The American College of Emergency Medicine Physicians (ACEP) publishes interpretations of the 2023 Evaluation and Management guidelines. Those have been utilized by most of the Revenue Cycle companies that deal with Emergency Medicine claims. However, different payers may interpret them differently, thus denials are generated and must be addressed. As we see payers taking a more militant approach in paying claims we see denials increasing for such things as “level 5” EM visits which can often be down coded to “level 4” and even “level 3”. We seldom see denials for critical care however we can often see denials for Evaluation and Management services with certain procedures. Payers are also prone to look at the final diagnosis for a claim rather than the reason for the visit which, in an Emergence Department can be significant. Therefore, when denials occur for lack of medical necessity, a favorite denial reason for payers, the chart must be reinterpreted and a reconsideration sent back to the payer.
The most significant thing to look for in a coding company is both internal and external auditing of their work. This not only gives the client a much higher level of satisfaction of accuracy but it also provides an opportunity for the coding company to see where their code assignment may differ and for what reasons. Again, Emergency Medicine Evaluation and Management (EM) coding can be very subjective and one needs to know where the subjectivity can create both inaccurate coding and payment issues. Finally, documentation is one of the most important elements of coding as coders select words and phrases from documentation to fit into the appropriate code descriptor boxes so to speak and assign the code.
If coding companies are not working with clients to notify physicians when documentation omissions create a down code or are not generally working with physicians to notify them of changes in documentation requirements, then it is a given that revenue would be affected. At Edelberg we have coined the phrase “Audication” and we have established an “Audication” program to stress the importance of education and audit of both physicians and coders. Physicians must be reviewed for their ability to assure documentation fulfills coding requirement for each level of service. Education of any deficiencies for both coders and providers is a concrete way to continue to address changes in the industry, changes within the institution for available medical record formats, and the ever changing coding world.
So the more pressing questions is how can you not afford to have a coding company as your expert on your team?…something like that😊
One of emergency medicine’s top issues today results from boarding patients in the emergency department while waiting for a Psychiatric bed or transfer to an outside Psychiatric facility. Although the evaluation and management codes apply for the initial evaluation and workup (99281-99285) or provision of ED Critical Care (99291-99292), services provided on subsequent days following the initial day of treatment come under a different set of codes when certain conditions are met. If the patient’s condition requires ongoing care in the emergency department while a decision is being made regarding appropriate disposition consider the following CPT codes when the definition fits the condition:
- Initial Hospital Inpatient or Observation Care (Initial ED Visit is billed separately with modifier -25) CPT 99221-99223)
- Subsequent Hospital Inpatient or Observation Care (99231-99233)
- Hospital Inpatient or Observation Care Services (Including Admission and Discharge Services) 99234-99236
- Hospital Inpatient or Observation Discharge Services (99238-99239)
NOTE: EACH SET OF OBSERVATION CARE ESTABLISHES TOTAL PER CODE SHOULD THE PROVIDER ELECT TO USE TIME INSTEAD OF MEDICAL DECISION MAKING TO DETERMINE THE OBSERVATION LEVEL. IF USING TIME TO DETERMINE THE OBSERVATION LEVEL, A CLEAR, CONCISE TIME STATEMENT MUST BE DOCUMENTED BY THE PROVIDER.
Although many practices follow Medicare guidance, the CPT Assistant, published by the AMA, addressed this policy in the July 2019 issue (page 10). The publication referenced that the Inpatient/Observation code set may be used to report these ED encounters. The initial day of care would be reported with 99281-99285, 99291-99292, or 99221-99223. The second day and subsequent days would be reported with a subsequent Inpatient/Observation Care code (99231-99233). If discharged, the final day of care would be reported using the Inpatient/Observation discharge day codes (99238-99239) or the Subsequent Inpatient/Observation Care codes if the patient is admitted or transferred.
As a national medical auditing company, Edelberg sees numerous examples of good and bad documentation practice so provider education is a key element to getting the coding right initially or, if the claim is denied, supporting the Observation services through detailed and thorough documentation. CMS requires a medical observation record for the patient which contains dated and timed physician orders for the observation services, nursing notes and physician progress notes while the patient is receiving observation services. This record must be in addition to any record prepared as a result of an emergency department or outpatient clinic encounter. In essence, the medical record for observation services should include the initial emergency department record supplemented with at least daily progress notes and a discharge summary.
The physician’s order to initiate observation status is critically important to officially “start” the Observation care process and ensure that Observation care is billed correctly. In the case of “psychiatric holds,” the ED provider is required to document the order to place the patient in observation status pending either transfer or admission to ensure that any additional days in the ED may be reported with the observation codes. To support subsequent observation care for the additional days waiting for disposition, the record should indicate that the patient is receiving active treatment from the ED provider and not simply being boarded pending transfer or admission.
In the complex landscape of healthcare, precision and compliance are paramount.
Medical coding is a crucial component of healthcare operations. It plays an important role in ensuring accuracy and adherence to regulatory standards.
This blog delves into the world of coding compliance in healthcare and why it’s indispensable.
Discover how Edelberg & Associates is revolutionizing this field with innovative coding compliance services.
What is Coding Compliance in Healthcare?
Web-Based Medical Coding Technology compliance in healthcare refers to the practice of accurately and consistently translating medical procedures, diagnoses, and services into
standardized codes.
This includes Current Procedural Terminology (CPT) and International Classification of Diseases (ICD) codes.
These codes are essential for various aspects of healthcare, including medical billing, reimbursement, and the maintenance of comprehensive patient records.
Coding compliance ensures that the codes assigned to medical services align with established regulatory standards and guidelines.
This alignment is critical for several reasons:
- Billing and Reimbursement. Accurate coding is vital for healthcare providers to correctly bill insurance companies or patients. Incorrect codes can lead to payment delays, denials, or overpayments.
- Medical Records. Accurate coding helps maintain precise and detailed medical records. This, in turn, supports effective patient care, facilitates research, and aids in healthcare decision-making.
- Audit Preparedness. Healthcare organizations must adhere to coding regulations to minimize the risk of audits and investigations. Coding compliance helps reduce the chances of billing errors and non-compliance with regulatory requirements.
- Legal and Financial Protection. Non-compliance with coding regulations can lead to legal and financial consequences for healthcare providers. Coding compliance helps mitigate these risks.
What is the Purpose of Coding Compliance?
The purpose of coding compliance in healthcare is multi-faceted and essential for the integrity and effectiveness of the healthcare system.
Here are the key purposes of coding compliance:
- Accurate Billing and Reimbursement. One of the primary purposes of coding compliance is to ensure that healthcare providers accurately bill for the services they provide. It helps prevent underbilling or overbilling, reducing financial discrepancies.
- Reduction of Billing Errors. Coding compliance aims to minimize billing errors, such as incorrect codes or code modifiers. Reducing errors helps healthcare providers avoid payment delays, denials, and audits. This can be costly and time-consuming.
- Enhanced Patient Care. Accurate coding is essential for maintaining precise medical records. These records are crucial for patient care.
- Mitigation of Legal and Financial Risks. Non-compliance with coding regulations can result in legal and financial consequences for healthcare providers. Coding compliance programs help identify and rectify coding errors. Reducing the risk of legal actions, fines, and penalties.
- Quality Assurance. Customized Auditing Programs often include quality assurance auditing and monitoring processes that help healthcare organizations identify areas of improvement. By continuously assessing coding accuracy and compliance, organizations can enhance the quality of their coding practices.
- Data Analysis and Research. Accurate coding is crucial for healthcare data analysis, research, and epidemiological studies. Researchers and public health officials rely on accurate coding to understand healthcare trends, track diseases, and make informed policy decisions.
- Regulatory Adherence. Healthcare is heavily regulated, and coding compliance ensures that healthcare providers adhere to these regulations. Compliance with coding guidelines and regulations is essential for maintaining the trust and credibility of healthcare institutions.
Demystify Coding Compliance with Edelberg & Associates
In the intricate world of healthcare, coding compliance safeguards patients’ well-being, optimizes billing and reimbursement processes, and shields healthcare providers from legal and financial pitfalls.
Edelberg & Associates, with its extensive experience and highly skilled management team, stands as a beacon of innovation in the coding compliance landscape.
Their commitment to affordable coding services and dedication to employing highly trained coding professionals sets them apart.
Edelberg & Associates’ pioneering approach to being the leader in medical coding compliance services saves time and money and ensures that accuracy and compliance remain at the forefront of healthcare operations.
Embrace the future of coding compliance with Edelberg & Associates, where innovation meets precision.
Your journey to coding excellence begins here.
Sexually transmitted infections (STI) consist of N. gonorrhoeae (gonorrhea) and C. trachomatis (Chlamydia) which are highly prevalent in the family of sexually transmitted disease (STD). There were nearly 68 million infections in 2018 (prevalence), and that 1 in 5 people in the U.S. have an STI. The graphic also shows that there were 26 million STIs acquired in 2018 (incidence). The direct lifetime medical costs of new STIs in 2018 totaled nearly $16 billion (in 2018 dollars). Gonorrhea is a common STI and the CDC estimates approximately 1.6 million new gonorrhea infections occurred in the United States in 2018 with more than half occurring among young people aged 15-24.[1] Chlamydia is also a common STD that infects both men and women and can cause serious permanent damage to a woman’s reproductive system making it difficult for her to get pregnant and can also cause a potentially fatal ectopic pregnancy.
Testing
Testing is key in the prevention of the spread of STDs in both men and women who are sexually active. Testing can be accomplished either through urine sample or cotton swab sample from the vagina. Persons with HIV infection should be screened annually if sexually active and more frequently (three-to-six month intervals) for men who have sex with men (MSM), particularly for those with multiple partners. Under-treatment and/or delayed treatment of an STD can and often does result in significant consequences for the patient. The transmission of an STD pathogen continues for the sexually active patient; complications of an untreated progressive infection can include pelvic inflammatory disease with risk of infertility, ectopic pregnancy and/or chronic pelvic pain. For the provider, there is no guarantee the patient will return, staff increases work-flow to contact patient for return for treatment, and neither patient or clinician are satisfied with the outcome.
In some cases the clinician elects to treat the patient before lab results are provided so the patient is treated for “possible” infection that may not be present thus resulting in unnecessary medication that may have adverse effects, chance of increasing antibiotic-resistant infections, loss of confidence in clinician’s decision making when treating a non-existent infection, additional strain on staff work flow to reschedule for correct treatment, and reduced patient and clinician satisfaction.
Treatment
According to the CDC, “in settings where same-day treatment is available for patients with STD-related conditions and for sex partners of patients with a diagnosed STD, treatment should not be delayed while awaiting diagnostic test results. Delays in treatment might increase complications and contribute to transmission of infection in the community; and same-day treatment has numerous public health benefits. In an STD specialty care setting, same-day treatment should take place on site with the provision of a full course of appropriate medication. The first dose should be administered while the patient is in the clinic.”
Insurance Coverage for Testing and Treatment
Medicare Part B (Medical Insurance) covers sexually transmitted infection (STI) screenings for chlamydia, gonorrhea, syphilis, and/or Hepatitis B if you’re pregnant or at increased risk for an STI. Medicare also covers up to two face-to-face, high-intensity behavioral counseling sessions if you’re a sexually active adult at increased risk for STIs. Each session can be 20-30 minutes long. Medicare covers STI screenings once every 12 months, or at certain times during pregnancy. Medicare covers up to two behavioral counseling sessions each year.
Private payers have individualized coverage based on employer options plan internal coverage options. According to the CDC, the affordable care act (ACA) includes provisions aimed at improving coverage of, and access to certain preventive health services. The following plans cover testing without cost-sharing.
- Non-grandfathered private health insurance plans
- Medicare
- Medicaid expansion plans (optional for adults, depending on state policy. Often covered for children)
- Traditional Medicaid plans
Overview of Relevant Reporting Codes
Preventive Medicine
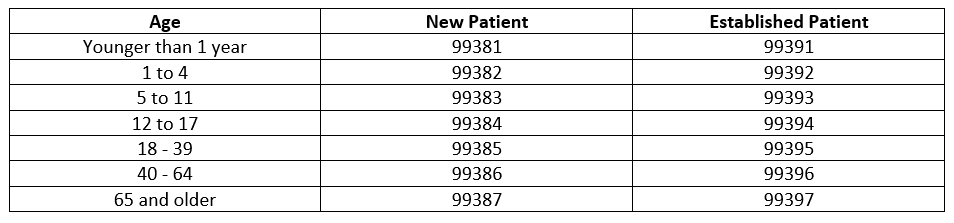
Preventive medicine codes (New 99381-99387), (Established 99391-99397) are used to report the preventive medicine evaluation and management of infants, children, adolescents, and adults. If an abnormality is encountered or a preexisting problem is addressed in the process of performing this service and it is significant enough to require additional workup requiring the key components of an E/M service, the office/outpatient codes should be reported with modifier -25 (CPT 2023).
2023 CODE TABLE; PREVENTIVE MEDICINE SERVICES
Documentation
Documentation by providers must include whether the patient is New or Established, age of patient, complete, pertinent history and physical examination, orders for testing and treatment, risk factors from findings, differential diagnoses if pertinent, and referral.
Diagnosis findings should be documented to include conclusions following testing, additional problems managed at the visit and co-existing problems either being managed concurrently by the treating physician or those that exist and will be managed on follow-up to another physician and/or specialist.
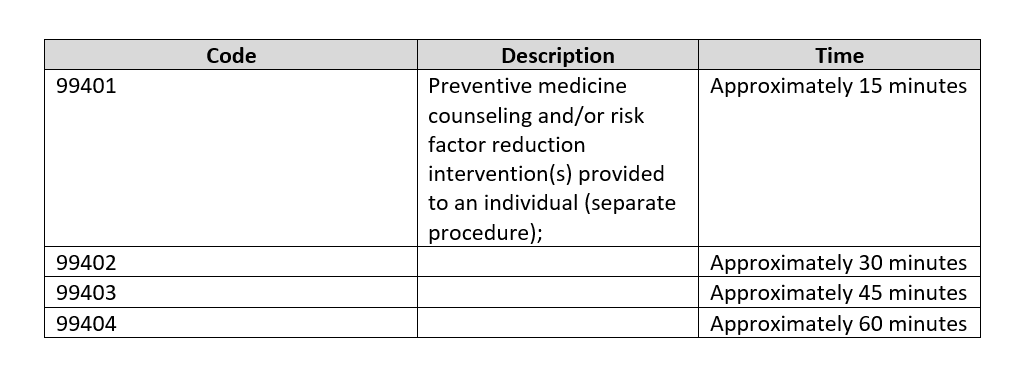
Counseling Risk Factor Reduction and Behavior Change Intervention
Counseling for Risk Factor Reduction and Behavior Change Intervention are used to report services provided face-to-face by a physician or other qualified health care professional for the purpose of promoting health and preventing illness or injury. If billed in addition to evaluation and management codes, the -25 modifier would be appended to the E/M level. See CPT 2023 for additional descriptors.
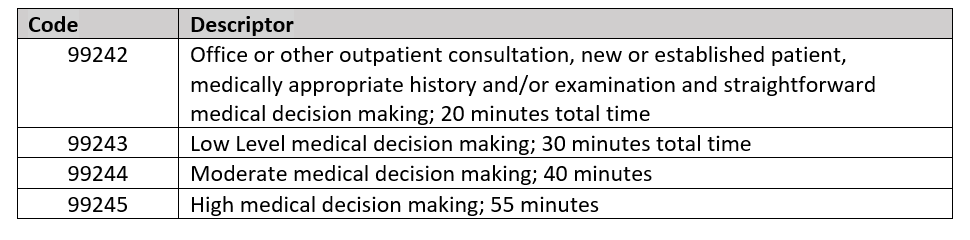
Counseling Codes for Office or Other Outpatient Consultations
Counseling codes can be used for the initial consultation for a specific problem when referred by another provider. Any follow-up services related to the specific problem provided by the consulting physician are billed with the appropriate outpatient visit codes.
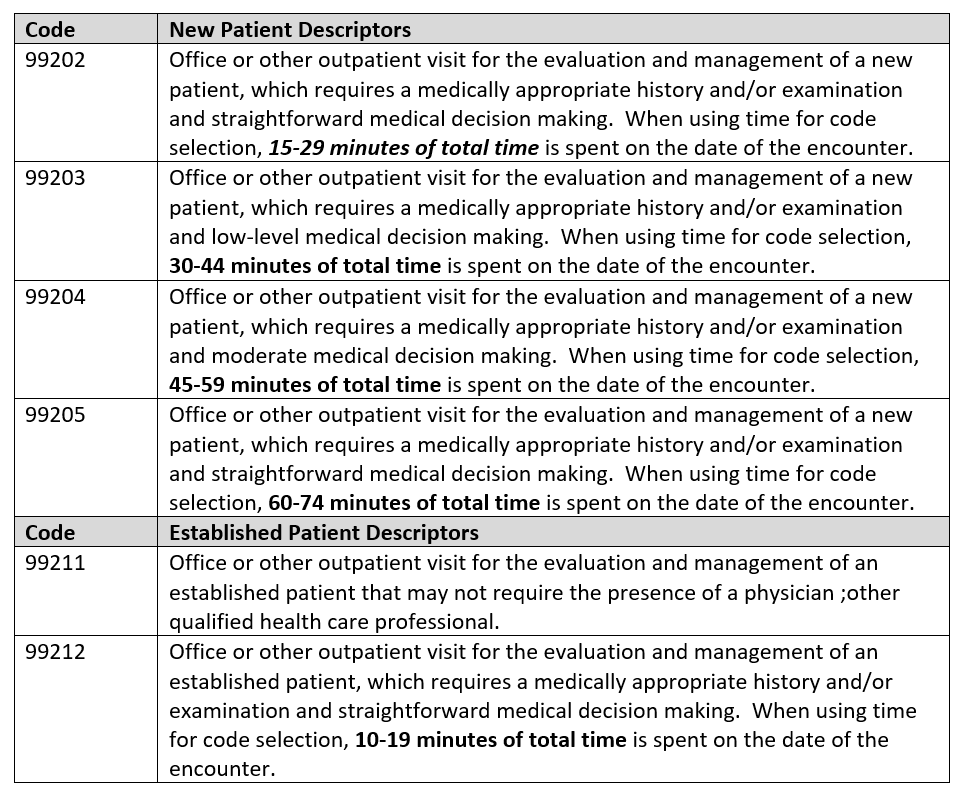
2023 Content of CPT Evaluation and Management Service Codes
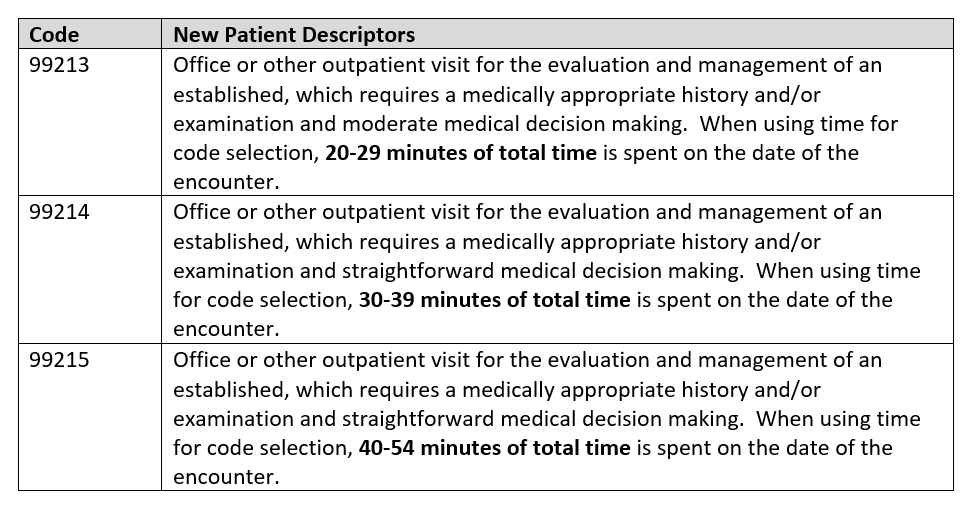
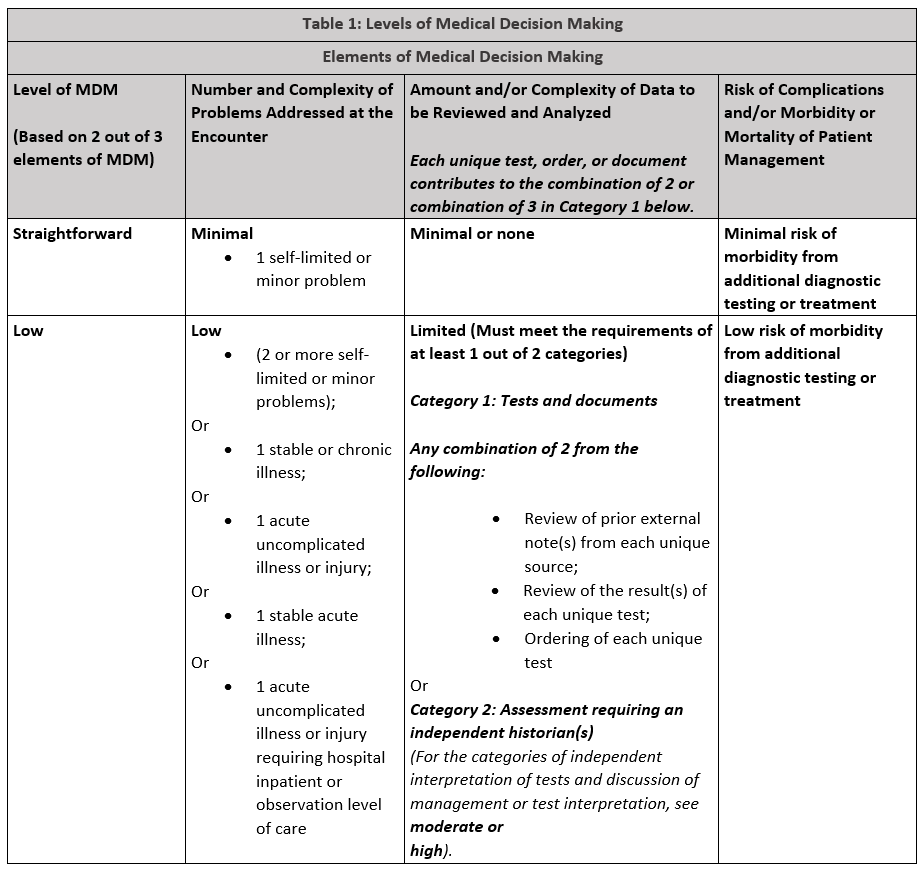
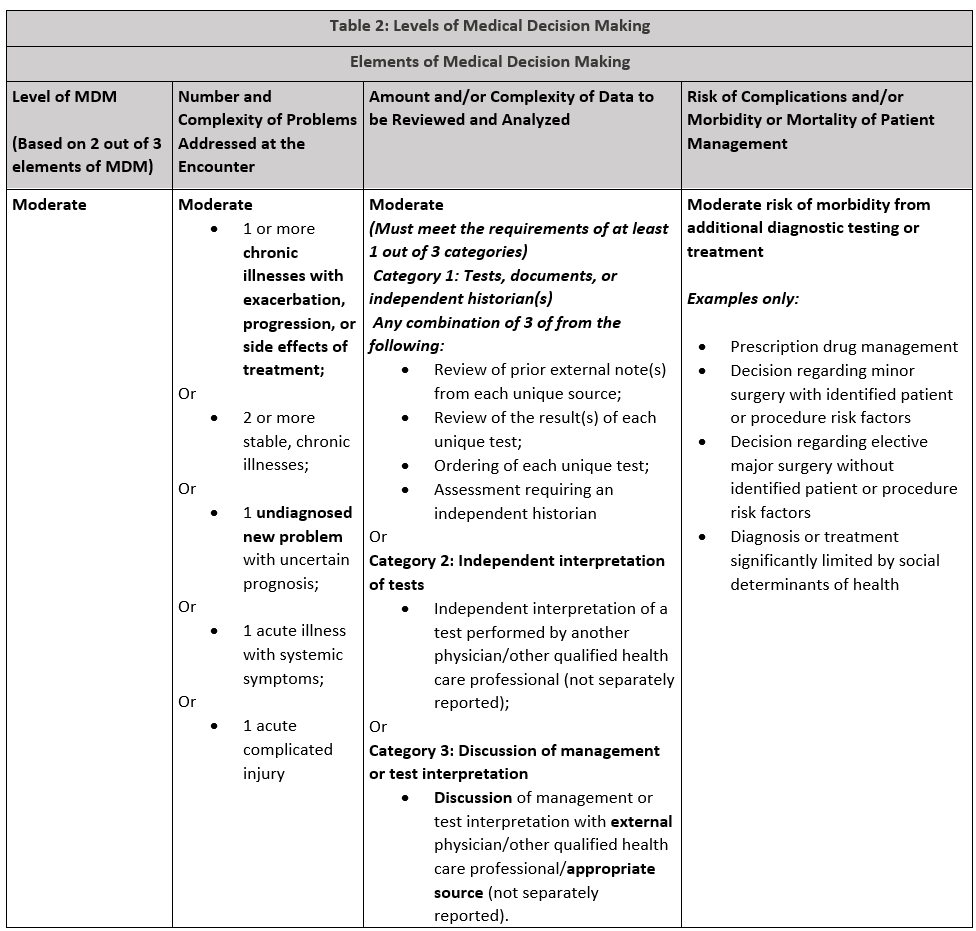
The E/M code descriptors were modified by the American Medical Association for revision in 2022 and 2023. There were extensive changes made in how the final code level is chosen which recognizes the level of Medical Decision Making or Time, depending on the code set, as the determinant of the code choice. History and Physical Examination are required to be “medically appropriate” but are not calculated in the final code choice. For outpatient office/clinic visits, either Medical Decision Making or Time determine the code billed. Times range from
New Patient
The CPT definition of “New Patient” is one who has not received any professional services from the physician or other Qualified Health Care Professional (QHCP) or another physician or QHCP of the exact same specialty and subspecialty who belongs to the same group practice withing the past three years.
Established Patient
The CPT definition of “Established Patient” is one who has received professional services from the physician or other qualified health care professional or another physician or other QHCP of the exact same specialty and subspecialty who belongs to the same group practice within the past three years.
Consideration of Time in E/M Levels
Time is not a consideration for coding emergency department E/M levels but it will be for most other E/M levels. Note the times listed in each table for appropriate time requirements must be supported by documentation in the medical record.
Office or Other Outpatient Services
Emergency Department Services
As of January 1, 2023, The emergency department evaluation and management codes to not distinguish new or established patients nor do they recognize total time spent on the date of the encounter. These codes are used by the emergency medicine provider scheduled in the ED. For other providers seeing patients in the ED, the office or other outpatient service codes are used. Emergency medicine evaluation and management levels are determined by two of three medical decision making components that meet or exceed the requirements of the level.
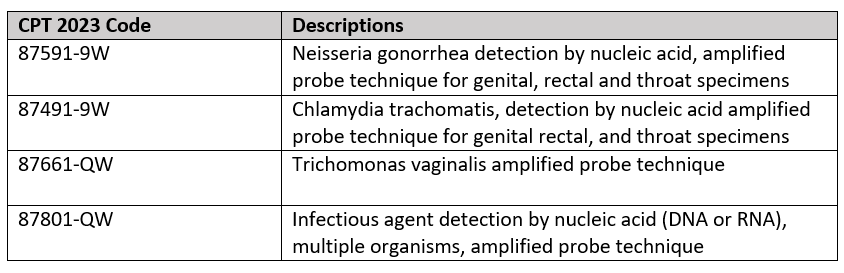
Selecting the appropriate Laboratory CPT Code
Whether or not the clinic bills independently for the labs used to diagnose chlamydia and gonorrhea specimens, it is important to assure the lab CPT codes are billed correctly. Following are codes pertinent to Gonorrhea and Chlamydia testing:
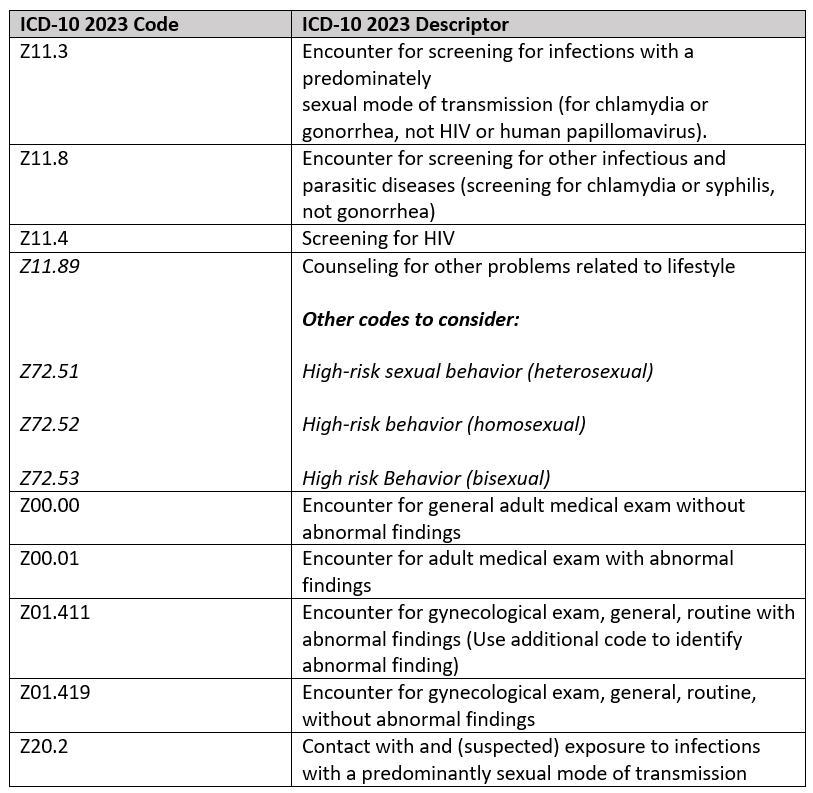
SELECTED STI SCREENING PREVENTIVE ICD-10 DIAGNOSIS Z-CODES 2023
According to the CDC in 2020, “Screening and diagnostic testing are important to detect asymptomatic or confirm suspected infections. Previous studies have documented that one third to one half of primary care clinicians routinely screen men or women for STDs (chlamydia, gonorrhea, syphilis, or HIV) (26,33,38,39). Obstetricians-gynecologists screen nonpregnant women more often than other primary care physicians (39–41). Community health centers often provide routine HIV testing for pregnant women but less frequently offer routine HIV testing for men and nonpregnant women (42,43). Some emergency departments perform routine HIV testing, although the practice is not widespread (44). For correctional settings, routine testing varies by type of facility. State and federal prison systems commonly perform routine syphilis testing at intake but less often offer routine testing for HIV, gonorrhea, or chlamydia (45). Some city and county prisons conduct routine testing for syphilis but rarely offer routine testing for HIV, gonorrhea, or chlamydia (45). Jails and juvenile detention centers infrequently offer routine testing for STDs and rarely perform routine HIV testing (46,47).”
Asymptomatic Coding for STI
The following codes identify STI screening and preventive diagnosis coding opportunities for 2023. Note some code descriptors have minimal changes from prior years. These codes are to be used for testing for a disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those that test positive for the disease. One cannot emphasize the importance of including ALL pertinent diagnosis codes to provide a total picture of the patients’ problems managed at the encounter.
Signs and Symptoms that Impact Coding for STDs
Often patients see their physician, go to an Emergency Department or Urgent Care Center complaining of symptoms consistent with an STD. Following are some of the complaints consistent with suspicion of STD:
For females:
- Genital itchiness
- Lumps and bumps in the vulva and vagina
- Changes in vaginal discharge
- Pain in the affected area
- Lower abdominal pain
- Pain during intercourse or urination
For males:
- Unusual discharge from the penis
- Lumps or bumps on the genital area
- Sores or ulcers on the genital area
- Burning or pain during urination
- Pain in the lower abdomen
- Pain during sex or ejaculation
- Painful or swollen testicles
These are visits that are billable based on the location where care is sought. For the Office, Codes 99202-99205 (New patient) or 99211 – 99215 (established patient) would be appropriate for the overall examination and treatment. The laboratory tests would be billed separately and assigned the code consistent with the type of test. If the site of service is the ED, Codes 99281-99285 would be appropriately billed by the provider and the hospital would bill for the technical service using the 99281-99282 codes as well as the laboratory codes.
Preventive Medicine Services (99381-99387) New patient, (99381 – 99397) Established patient, are examinations without symptoms but scheduled to identify risks and prevent a number of conditions. For example, a patient who is notified they have been exposed to an STD. Once a condition is identified during the preventive Medicine visit, labs may be ordered and additional visits may be necessary. When this occurs, the next visit would cease to be preventive and fall under the appropriate Office or Urgent Care service level and any labs would be billed separately.
Counseling Risk Factor Reduction and Behavior Change Intervention (Preventive Medicine, Individual Counseling (99401 – 99404) are time-based codes used to promote health and prevent illness or injury. These codes are used for individuals without a specific illness for which the counseling might otherwise be used as part of treatment. They would include family problems, diet and exercise, substance use, sexual practices, injury prevention, dental health and diagnostic and laboratory test results available at the time of the encounter for review and discussion.
Coding Technique Example
20 year-old college student known to the practice schedules a visit with concerns relating to unprotected sex recently. Patient collects a vaginal swab sample testing is performed prior to the exam. Patient is examined including pelvic examination. Exam and on-site STI lab results indicate patient is positive for Chlamydia. Results reviewed with patient then patient received ceftriaxone (Rocephin) 250 mg given intramuscularly and Azithromycin (Zithromax) is given orally. Patient is counseled and advised to return for recheck in ten days.
Codes Assigned
CPT Procedure Codes:
99204-25 New patient office service
87801 Infectious agent, multiple organisms
96372 Therapeutic, prophylactic, or diagnostic injection (specify substance or drug); subcutaneous or intramuscular.
XXXXX Identify the substance injected
ICD-10 Diagnosis Codes:
Z70.2 Other specified counseling
Z11.3 – Encounter for screening for infections with a predominately sexual mode of transmission
Z72.51 High risk sexual behavior (heterosexual)
Example 2:
22 year-old female admits to unprotected sex 1 week ago and wants to be tested for STD although asymptomatic at this time. Patient is currently homeless. Patient conducts self-collected swap on arrival. Physical examination includes pelvic examination and STI panel is positive for Trichomonas. Patient is prescribed metronidazole (Flagyl®), counseled on prevention and discharged. Provider spends 35 minutes in attendance to the patient including counseling and discussion of lab results.
CPT Procedure Codes
99204-25 New patient office service (undiagnosed new problem with uncertain prognosis, prescription drug management; treatment significantly limited by social determinates of health (homelessness, inability to afford medication)
87801 Infectious agent, multiple organisms
ICD-10 Diagnosis Codes:
A59.00 -Urogenital trichomoniasis, unspecified
Z11.3 – Encounter for screening for infections with a predominately sexual mode of transmission
Z72.51 High risk sexual behavior (heterosexual)
K62.89 Other specified counseling
References and Additional Reading:
Gonorrhea-CDC Detailed Fact Sheet: https://www.cdc.gov/stdfact-gonorrhea-detailed.htm
CDC STD Fact Sheets: https://www.cdc.gov/std/healthcomm/fact_sheets.htm
CDC: Sexually Transmitted Disease Preventive Services Coverage: https://www.cdc.gov/std/healthcomm/fact_sheets.htm
Medicare/CMS: https://www.medicare.gov/coverage/sexually-transmitted-infection-screenings-counseling
CDC Sexually Transmitted Diseases: https://ww.cdc.gov/nchhstp.newsroom/2021/2018-STI-Incidence-prevalence-estimates.html.
CDC: https://www.chlamydiaexplained.com/what-is-the-best-treatment-for-gonorrhea-and-chlamydia/
Drugs.com: https://www.drugs.com/medical-answers/antibiotics-treat-chlamydia-gonorrhea-3121689/
National Library of Congress: Diagn Microbiol Infect Dis. 1993 Feb;16(2):165-72. doi: 10.1016/0732-8893(93)90016-z.
Chlamydia trachomatis by Amplified Probe Technique: https://www.uwhealth.org/lab-test-directory/microbiology/name-67808-en.html; UWHC Laboratory Services: Microbiology
Trichomonas Facts: https://www.cdc.gov/std/trichomonas/STDFact-Trichomoniasis.htm
STD Treatment: https://www.cdc.gov/std/treatment/default.htm
CDC Trichomoniasis Treatment: https://www.cdc.gov/std/treatment-guidelines/trichomoniasis.htm
Trichomoniasis Treatment: https://my.clevelandclinic.org/health/diseases/4696-trichomoniasis
ICD-10 Data: https://www.icd10data.com/ICD10CM/Codes/A00-B99/A50-A64/A59-/A59.9
CPT 2023: Professional Edition, American Medical Association; Copywrite 2022
Chlamydia testing and treatment: https://www.chlamydiaexplained.com/
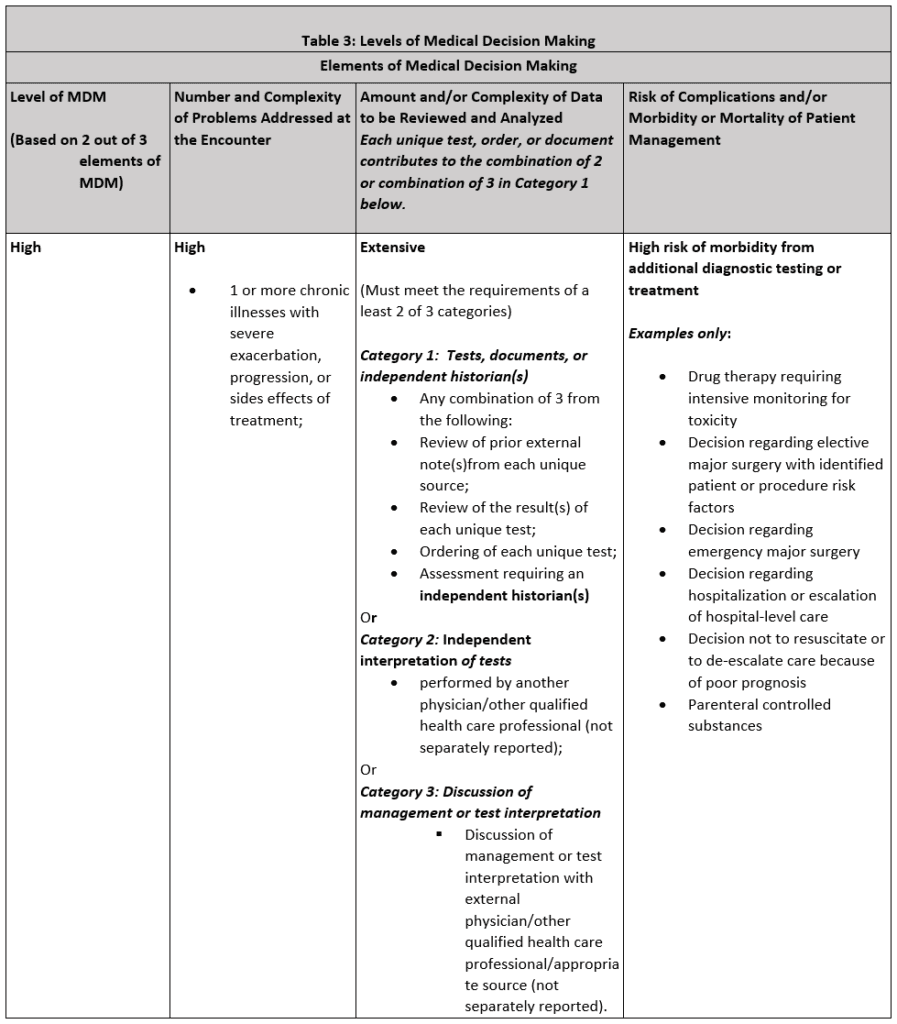
As we closed the first month of the new 2023 E/M Coding Guidelines for emergency medicine, a number of identified issues arose which will require provider attendance to documentation details on a much larger scale. We noted at some facilities a drop in the percentage of 99285’s that could not be fully offset by the increase in 99283’s. So, now is a great time to recap what is required for 99285!
Nature of Presenting Problem:
1 or more chronic illnesses with severe exacerbation, progression, or sides effects of treatment
Amount and/or Complexity of Data to be Reviewed and Analyzed – Extensive
(Must meet the requirements of a least 2 of 3 categories)
Category 1: Tests, documents or independent historian(s)
Any combination of 3 from the following:
- Review of prior external note(s)from each unique source;
- Review of the result(s) of each unique test;
- Ordering of each unique test;
- Assessment requiring an independent historian(s)
Or
Category 2: Independent interpretation of tests
- Performed by another physician/other qualified health care professional (not separately reported);
Or
Category 3: Discussion of management or test interpretation
Discussion of management or test interpretation with external physician/other qualified health care professional/appropriate source (not separately reported)
High risk of morbidity from additional diagnostic testing or treatment
Examples only:
- Drug therapy requiring intensive monitoring for toxicity
- Decision regarding elective major surgery with identified patient or procedure risk factors
- Decision regarding emergency major surgery
- Decision regarding hospitalization or escalation of hospital-level care
- Decision not to resuscitate or to de-escalate care because of poor prognosis
- Parenteral controlled substances
Documentation Tips:
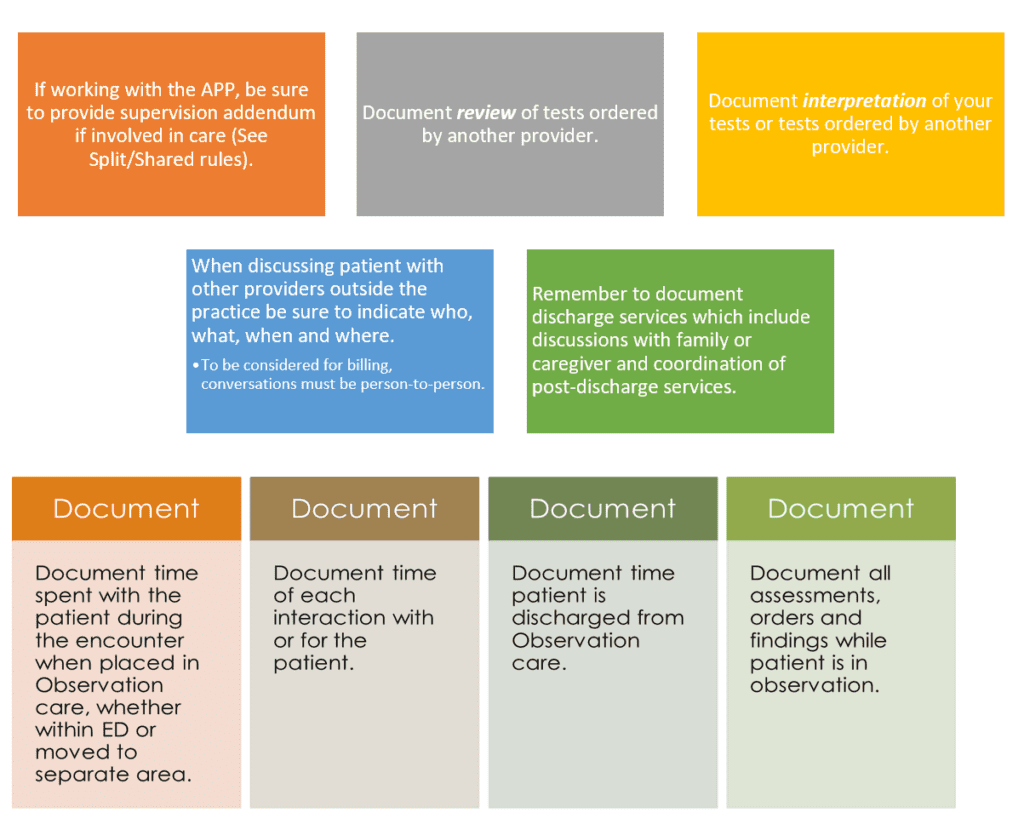
Some Documentation Take-Aways
- Do document differential diagnoses from which the final diagnosis is selected;
- Do document any social determinants of heath that may affect your treatment, disposition, patients ongoing health, etc.
- Do document the details of your discussions (interactive exchange) with other emergency physicians. Discussions with external physicians (from other specialties/other practices) should also be detailed in your documentation.
- Do reference any analysis (included in the thought processes for diagnosis, evaluation, or treatment) of a test vs. interpretation unless interpretation is coded separately. Any test or interpretation coded separately is NOT included in the E/M code level.
- Do provide content of any discussion with family, friends, caregivers, etc. (eg, parent, guardian, surrogate, spouse, witness who provides a history in addition to a history provided by the patient who is unable to provide a complete or reliable history (eg, due to developmental stage, dementia, or psychosis)
- Do develop rule-out/rule-in discussion from HPI/CC/Test results.
- Do use adjectives to describe patient condition, reasons for additional care, etc. (severe, significant, high risk, limited mobility, serious, altered, etc.
- Do remember to document time managing patient care for critical care.
- Do address any additional problems you identify and discuss how they are being managed e.g. diagnostic studies, differential dx, discussion with other providers, etc.
- Do not reference review of tests not ordered or performed, e.g. “ I have reviewed all tests and have discussed with patient and/or family.” Avoid generalized or templated statements if they are not pertinent or accurate.
© 2025 - Edelberg & Associates

